Mucormycosis (Black fungus) and COVID 19.
Discover Mucormycosis: a rare fungal infection exacerbated by India’s second wave of COVID-19. Learn more about its risks.
Catastrophic second wave of COVID 19 has left millions of people infected and dead. India is experiencing the world’s worst outbreak with not only rising COVID cases but also an alarming upsurge in a rare and potentially life-threatening fungal infection, Mucormycosis.
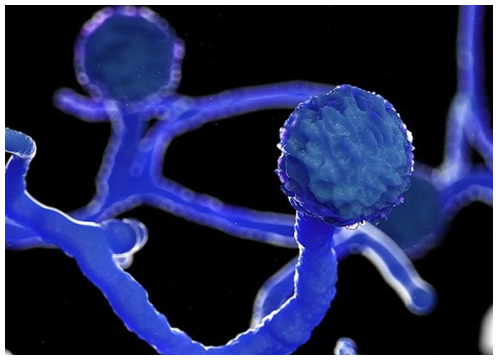
What is Mucormycosis?
According to CDC, Mucormycosis (black fungus) is a serious and rare fungal infection caused by a group of molds called mucormycetes. These fungi live in the environment, particularly in soil and in decaying organic matter, such as fruits, vegetables, leaves, compost piles, or rotten wood. People can contract mucormycosis by coming in contact with the fungal spores in the environment. For example, by inhalation of spores, by swallowing spores. Additionally, mucormycosisis likely to develop on the skin when fungus enters the skin via scrape, cut, burn, or any other type of skin trauma or injury.
How is mucormycosis related to COVID 19?
This rare fungal infection usually affects people who suffer from long-term health issues and/or take medications that lower immunity. Mucormyosis can be life-threatening in diabetics and immunocompromised individuals, such as recipients of organ or stem transplants, long-term usage of steroids, post-surgery, cancer.
When diabetes is poorly controlled, and blood sugar is high the tissues become relatively acidic, it creates a suitable condition for Mucorales fungi to grow. This has been identified as a risk factor for mucormycosis in India. People with diabetes and obesity are expected to develop more severe Covid-19 infections. This means they’re more likely to receive corticosteroids, which are frequently used to treat Covid-19. But corticosteroids together with diabetes increase the risk of mucormycosis. Meanwhile, coronavirus can damage airway tissue and blood vessels, which could also increase susceptibility to fungal infection.
Moreover, damaged lungs and suppressed immune system as seen in the case of COVID-positive patients make sinuses and nose the most common site of mucormycosis manifestation. From there it can spread to the eyes, leading to blindness, or the brain, causing headaches, seizures, stroke, and even death in certain cases. A recent study showed 94% of people infected with mucormycosis had diabetes and poorly controlled diabetes in 67% people.
Furthermore, long-term ventilation reduces immunity and there are speculations of the fungus being transmitted by the humidifier water being given along with oxygen.
Is it contagious?
No, it’s not. It does not spread from one person to another.

What are the symptoms?
You must visit your doctor if you experience the following symptoms;
- Cough
- Shortness of breath
- Fever
- Headache
- Nasal congestion, discharge.
- Sinus pain
- Blackened skin tissue
- Blisters
- Redness and swelling
- Ulcers
- One side facial pain
- Loosening of teeth
- Blackish discoloration over the bridge of the nose
How is mucormycosis treated?
This includes antifungal medication, controlling blood sugar, urgent removal of dead tissue.
The outcome is poor in many patients affected with mucormyosis. Nearly half of the patients affected will die and many will sustain permanent damage to their health.
Can we prevent mucormycosis?
Yes, mucormycosis can be prevented. Vaccination can help, it will protect from infection, which in turn will protect immunity. A strong immunity system can keep mucrmycosis at bay. Awareness must be created regarding fungal infections, diagnose them early, along with a focus on controlling diabetes and using corticosteroids wisely.

